St. Louis Children’s Hospital is one of the premier children’s hospitals in the United States and serves as the pediatric teaching hospital for anesthesia residents and fellows at Washington University School of Medicine in St. Louis.
The Division of Pediatric Anesthesiology at Washington University School of Medicine provides anesthesia and critical care services at St. Louis Children’s Hospital. St. Louis Children’s Hospital is a Level I Pediatric Trauma center with 455 pediatric beds and is one of the top pediatric transplant centers in the country. The hospital is consistently ranked among the best children’s hospitals in the nation and serves as the pediatric teaching hospital for anesthesiology residents and fellows at the School of Medicine.
Annually, St. Louis Children’s receives approximately 275,000 patients, with around 50,000 of them coming by way of the emergency department. Some of the major facilities include 15 operating suites, a 77‐bed PICU with 31-bed Heart Center and a 150-bed Level 4 NICU.
Approximately 20,000 anesthetics are administered each year to children of all ages, surgical conditions, and severity of illness. All surgical subspecialties are represented, including cardiac surgery, organ transplantation, orthopedic surgery, and major craniofacial surgery. We also provide a full range of diagnostic and therapeutic acute and chronic pain services, including both postoperative pain management and outpatient clinics, as well as two St. Louis Children’s Specialty Care Centers (West County and South County).
Washington University School of Medicine’s medical campus is located in the historic Central West End community of St. Louis, across the street from Forest Park, one of the largest urban parks in the nation. Forest Park is home to the St. Louis Zoo, St. Louis Science Center, the History Museum and the Art Museum. The medical campus is also a short distance away from the Missouri Botanical Garden, St. Louis Arch, and Laclede’s Landing.
Pediatric Anesthesia Fellows Bootcamp
Saturday, Feb. 8, 2025
St. Louis Children’s Hospital, Washington University School of Medicine in St. Louis
Follow us on Instagram!

See why we
love St. Louis!

Our Team
The fellowship is directed by Dr. Ashley Weinhold. Our pediatric faculty have diverse training backgrounds with the majority having board certification in pediatric anesthesiology and many with certification in pediatrics, emergency medicine, and medicine. Our research interests are primarily clinical and educational research.
Our faculty are all members of the Department of Anesthesiology who provide clinical services for anesthesia at St. Louis Children’s Hospital. Our anesthesia and pain services include the provision of inpatient and ambulatory anesthesia for infants and children in the general operating rooms, at locations within St. Louis Children’s including diagnostic radiology, interventional radiology, and the cardiac catheterization laboratory. In addition, we service satellite locations on our BJC medical campus (radiation and proton therapy, intraoperative MRI). In addition, there are two Children’s Specialty Care Centers—West County and South County—which both operate as outpatient surgical centers in a free-standing ambulatory center to serve the surrounding community.
The Fellowship Experience
The Pediatric Anesthesiology Fellowship program at Washington University School of Medicine is a one-year program with five available positions each year. During the 12-month program, fellows rotate through various rotations including general anesthesia, acute pain management and regional anesthesia, cardiac anesthesia, pediatric critical care, and ambulatory anesthesia. In addition, fellows also have 2 weeks of elective time. Fellows will have the opportunity to take care of complex NICU patients, stabilize trauma patients, participate in fetal surgeries, and take care of children receiving organ transplants (kidney, liver, heart, lung and combined transplants) in addition to caring for children coming in for
both outpatient procedures and complex surgical operations. By the time a fellow has reached the end of their year at St. Louis Children’s Hospital, they will have truly seen it all.
Adult & Pediatric Pain Dual Fellowship Opportunity
The Department of Anesthesiology and Washington University School of Medicine, together with Barnes-Jewish Hospital and St. Louis Children’s Hospital, also sponsor an ACGME-accredited fellowship in Anesthesiology Pain Medicine. There is now an option for a pediatric-focused track through this training program. The fellow on this combined track will care for both children and adults experiencing acute and chronic pain. Learn more
Each block is 4 weeks; 13 blocks total.
- 6 blocks of general pediatric OR, including designated time in non-operating room anesthesia
- 2 blocks of pediatric cardiac anesthesia (divided into four 2 week rotations)
- 2 blocks of pediatric acute pain management, regional anesthesia, and difficult airway service
- 0.5 blocks of pediatric critical care
- 0.5 blocks of elective
- 1 block of ambulatory pediatric anesthesia
- 1 block of Pediatric anesthesiology Education for Attending Readiness and Leadership (PaEARL) (time spent in perioperative care of pediatric patients)
Fellows have opportunities to pursue research activities, collaborate with faculty, and present at division conferences. Fellows are strongly encouraged to submit their work to national conferences, particularly the annual Society for Pediatric Anesthesia meeting. The division offers travel funds for fellows to attend the annual SPA conference if they have submitted an abstract. They also have the opportunity to collaborate with faculty and co-fellows on Quality Improvement (QI) projects within the division.
Faculty are highly involved in all aspects of the program. Our division faculty include recognized experts in pediatric cardiac anesthesiology, pain management, and patient simulation education. Fellows are paired with a faculty mentor within the first two months of fellowship to assist with career guidance and matriculation through the program.
The program has strived to keep fellow education at the forefront of the training experience. To that end, there are several unique educational experiences that are offered to our fellows:
- Pediatric Anesthesia Curriculum Review Series (PACRS) – developed by Drs. Young and Weinhold to serve as a pediatric anesthesiology board review curriculum for fellows, this program utilizes a flipped classroom approach to review topics from the ABA content outline followed by a weekly in-person interactive meeting with faculty.
- Fellows as Clinical Educators (FACE) – prioritizes the acquisition of skills in delivering effective feedback, bedside teaching, active learning methods, and other essential aspects of clinical education.
- Workshops – fellows participate in hands-on workshops covering regional anesthesia (including scanning with live pediatric models), vascular access, one lung ventilation, and other important topics.
- Cadaver lab – fellows participate in an adult cadaver lab specifically reviewing neuraxial techniques and fluoroscopic guided neuraxial techniques.
- Simulation – the campus has multiple state-of-the-art simulation labs. Fellows participate in simulation scenarios multiple times throughout the year to aid in the learning and evaluation process.
- Pediatric Anesthesia Fellows Bootcamp – a collaborative effort among fellows and experienced faculty across the nation providing intermediate-level knowledge and skills for mid-year pediatric anesthesia fellows.
- Oral Board Prep – fellows receive dedicated didactics and preparation for the ABA Applied Boards by meeting weekly with faculty from January to March and participating in mock exams.
- Division conferences – the division has weekly conferences that include topics such as Journal Club (monthly), M&M (monthly), faculty presentations and other invited guest speakers. Fellows also participate in morning conference by presenting during the year.
- Departmental Grand Rounds (weekly)
Stipends (July 1, 2024-June 30, 2025)
| PGY Level | Annual Stipend |
| PGY 1 | $67,808 |
| PGY 2 | $70,816 |
| PGY 3 | $73,679 |
| PGY 4 | $76,999 |
| PGY 5 | $80,372 |
| PGY 6 | $82,839 |
| PGY 7 | $86,568 |
| PGY 8 | $90,455 |
| PGY 9 | $94,531 |
Fiscal
- Moving stipend
- Board exam stipend
- Discretionary fund for professional expenses
- Paid parking
- Retirement plan with 2% University contribution
- Meal tickets when on call
- Monthly wellness funds
Travel
- SPA conference travel and registration funding with abstract submission
- Travel funding to attend a training bootcamp at a partnering institution
Insurance/Assistance
- Medical, Dental, Vision, and Pharmacy insurance benefit
- Life, Accident, and Disability insurance benefit
- Assistance with fertility treatment
- Access to WU Care and Employee Assistance Program (EAP)
- Assistance with child-care
Materials
- iPhone provided for professional use during fellowship
- White coat and departmental jacket
- Pediatric anesthesiology textbooks
- Precordial stethoscope
Professional
- Professional liability coverage
- Temporary medical licensure registration
- Temporary BNDD registration
Misc
- Fellows receive 15 vacation days, 5 floating vacation days, and up to 5 meeting days (to attend conferences etc.)
- Nonclinical time to work on their QI and scholarly projects.
- Fellow membership in the Society for Pediatric Anesthesia (SPA)
- PALS certification
- Cafeteria discount
- Access to Becker Library for trainee research and educational needs
For details regarding insurance and other benefits, visit hr.wustl.edu/benefits/change/hire/clinical-fellows-trainees.
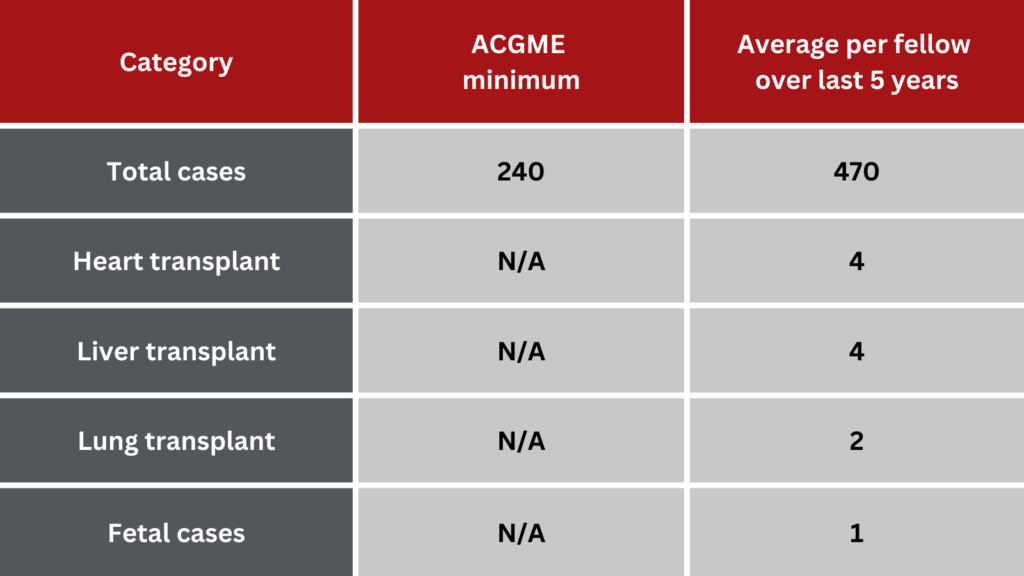
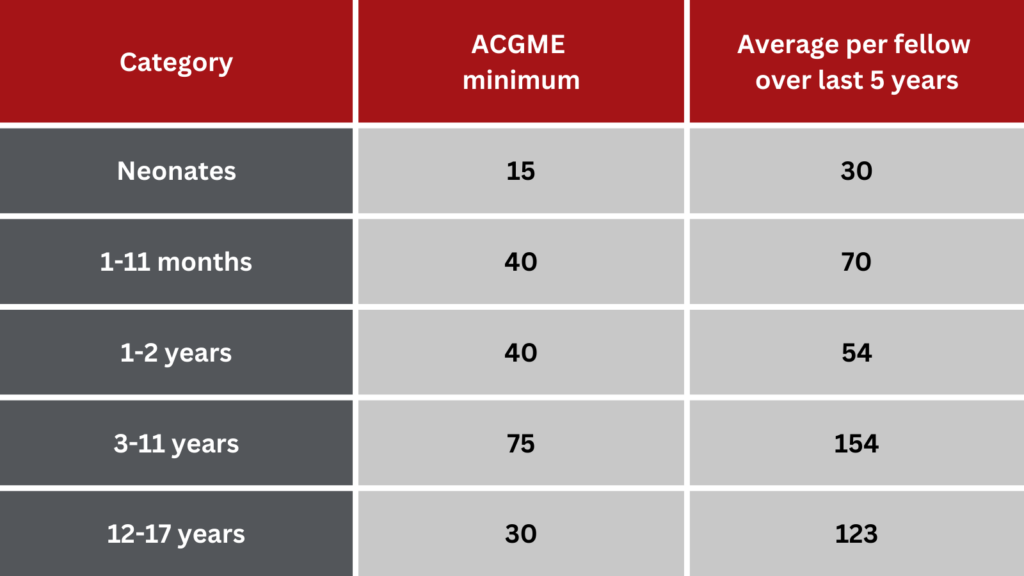
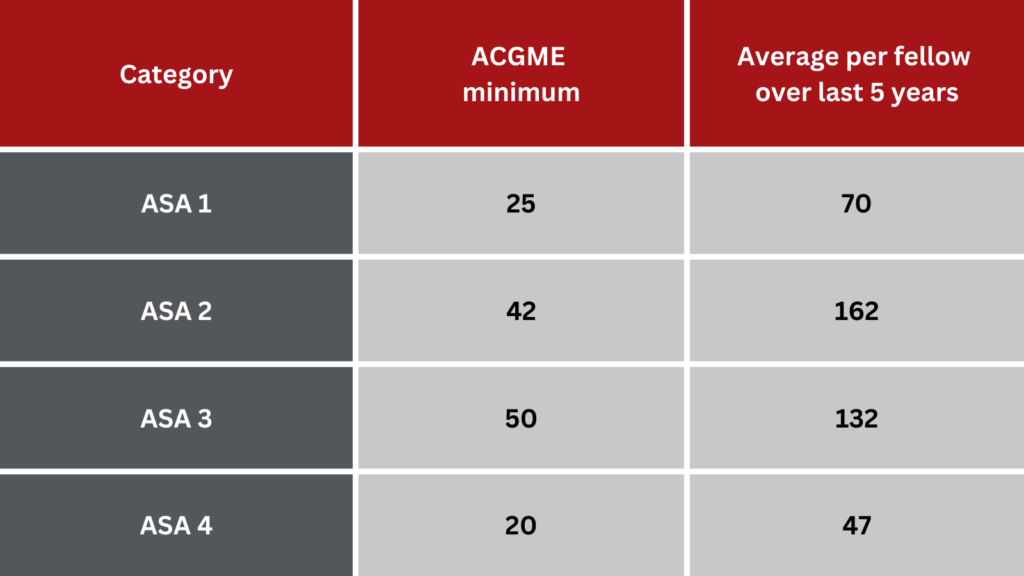
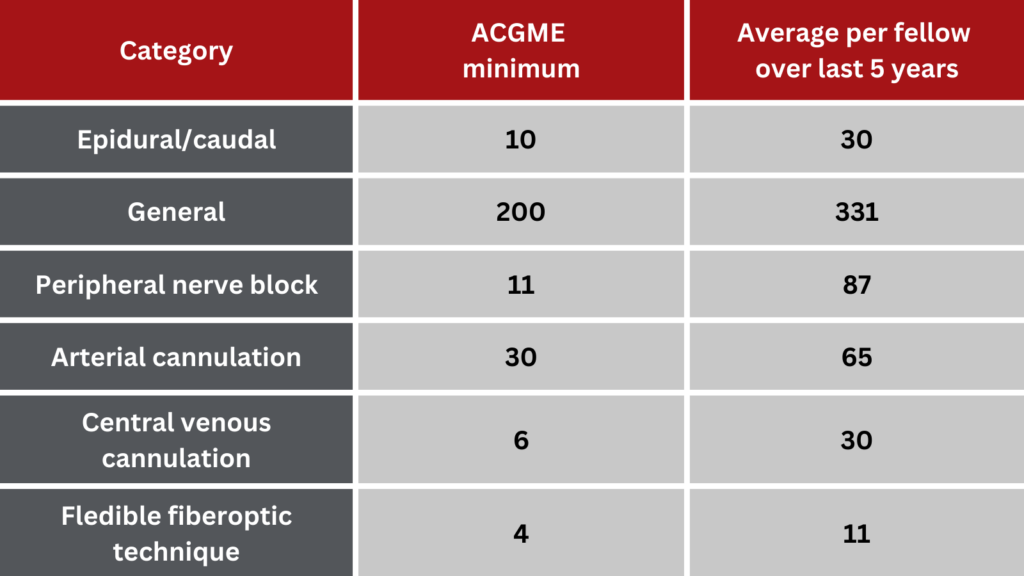
Case Logs
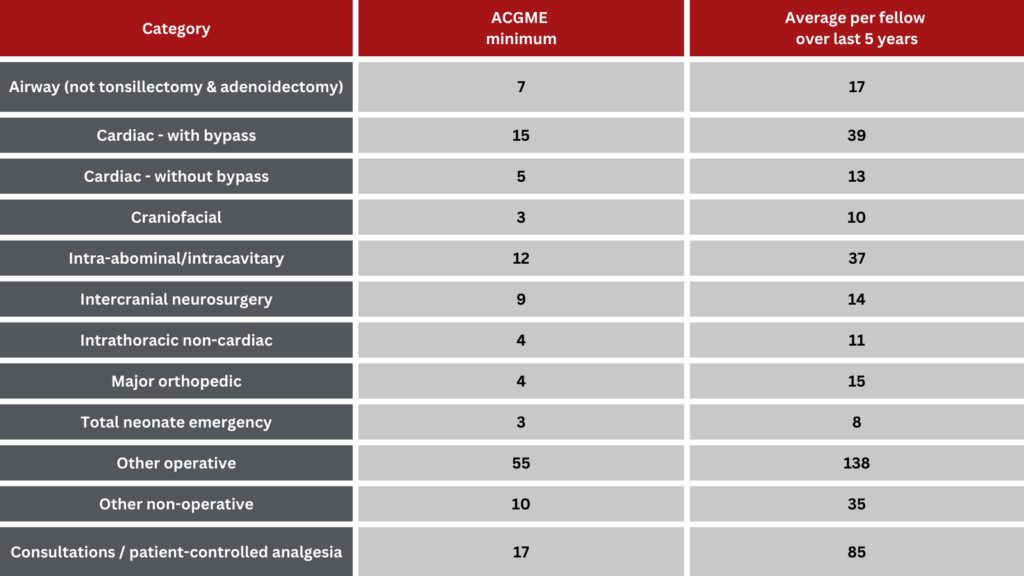
At the WashU Pediatric Anesthesiology Fellowship program, our fellows participate in diverse and challenging cases in line with ACGME requirements.
In FY 23, our division administered over 20,000 anesthetics and conducted over 5,000 inpatient pain visits. One thing that sets us apart is our commitment to individualized learning – fellows do not share index cases or other cases with co-fellows. This prepares them to emerge as skilled and independent consultant pediatric anesthesiologists.
Here’s how our fellow case numbers compare to the ACGME case minimums: